Mouth ulcers, also known as canker sores, are painful lesions that can occur in the oral cavity, affecting a person’s ability to eat, speak, and maintain oral hygiene. Understanding the causes, symptoms, and treatments of mouth ulcers can help you manage this uncomfortable condition effectively. In this blog, we will delve into the definition and types of mouth ulcers, common causes, symptoms, self-care treatments, and when it is necessary to seek professional help.
Definition and Types of Mouth Ulcers
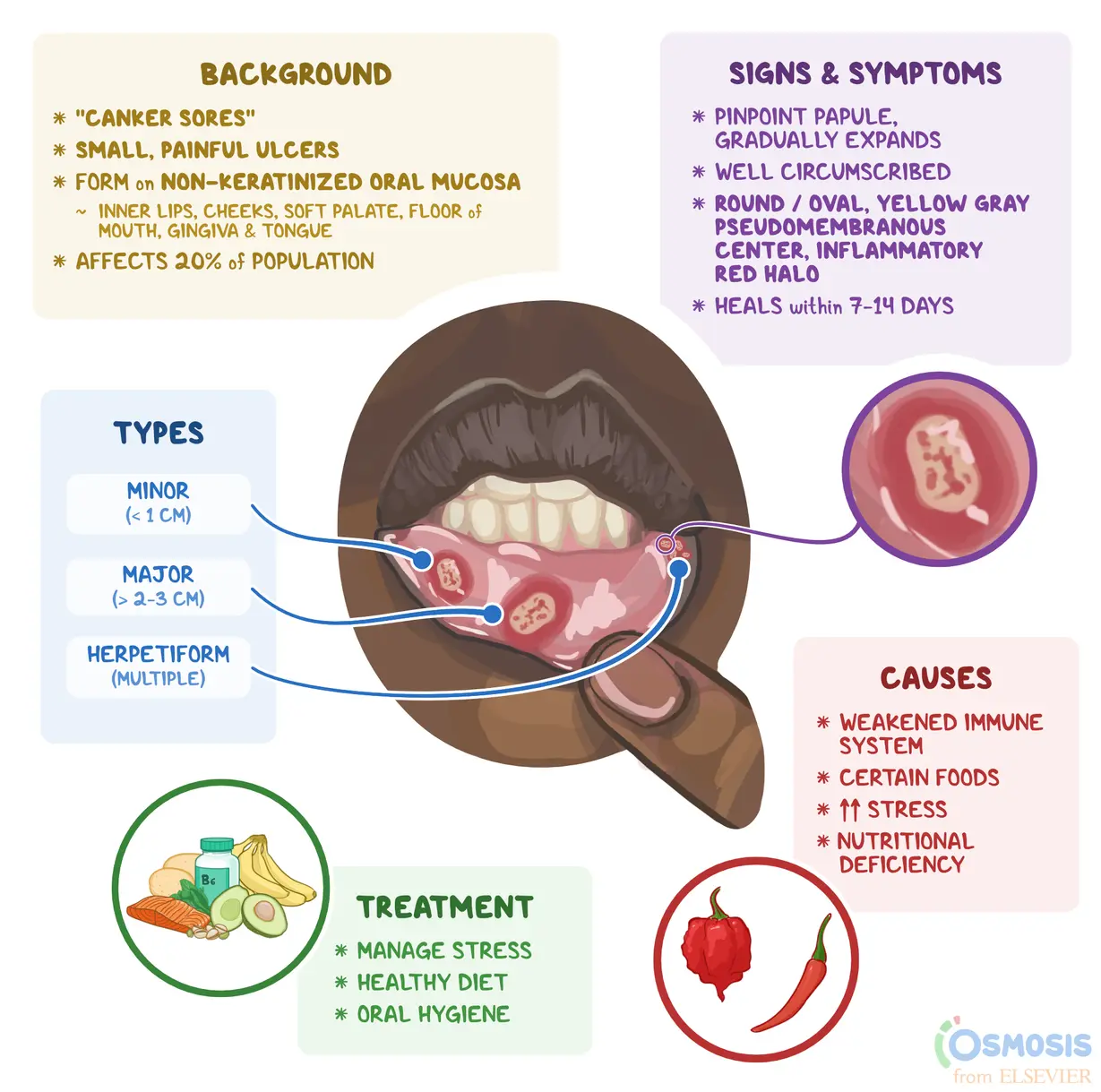
Mouth ulcers are small, painful sores that develop on the soft tissues inside the mouth, including the tongue, inner cheeks, gums, and the roof or floor of the mouth. They are usually shallow, round, and white or yellowish in color, surrounded by a red halo. There are several types of mouth ulcers, including:
- Aphthous Ulcers: The most common type, these canker sores are usually small and shallow, often occurring in clusters. They are not contagious and can recur frequently.
- Herpetic Ulcers: Caused by the herpes simplex virus, these ulcers often appear as clusters of small blisters and are contagious. They usually occur on or around the lips but can also appear inside the mouth.
- Traumatic Ulcers: These ulcers develop as a result of injury or irritation, such as biting the inside of the cheek, dental work, or abrasive foods.
- Other Ulcers: Less common types may be associated with underlying health conditions, such as Behçet’s disease, inflammatory bowel disease (IBD), or certain vitamin deficiencies.
Common Causes of Mouth Ulcers
Mouth ulcers can arise from a variety of factors, including:
- Injury or Trauma: Biting the inside of the cheek, irritation from dental appliances, or rough edges of teeth can lead to ulcer formation.
- Certain Foods: Acidic, spicy, or abrasive foods (like citrus fruits, nuts, and chips) can trigger or worsen mouth ulcers.
- Stress: Emotional stress can compromise the immune system, making individuals more susceptible to developing ulcers.
- Hormonal Changes: Hormonal fluctuations during menstruation or pregnancy can increase the likelihood of mouth ulcers in some individuals.
- Nutritional Deficiencies: Lack of essential vitamins and minerals, particularly vitamin B12, folate, iron, and zinc, can contribute to ulcer formation.
- Underlying Health Conditions: Certain medical conditions, such as autoimmune disorders or gastrointestinal diseases, can predispose individuals to develop mouth ulcers.
Symptoms and Self-Care Treatments
Symptoms of mouth ulcers may vary but commonly include:
- Painful sores or lesions in the mouth
- Burning or tingling sensations before the ulcer appears
- Difficulty eating, drinking, or speaking due to pain
- Swelling and redness in the affected area
While most mouth ulcers heal on their own within one to two weeks, self-care treatments can help alleviate discomfort and promote healing:
- Saltwater Rinse: Rinsing your mouth with warm saltwater can help reduce inflammation and promote healing.
- Topical Treatments: Over-the-counter gels or ointments containing benzocaine can provide temporary relief from pain and discomfort.
- Avoid Irritating Foods: Steer clear of spicy, acidic, or abrasive foods that can exacerbate ulcer pain.
- Maintain Oral Hygiene: Use a soft-bristled toothbrush and practice good oral hygiene to prevent infection and further irritation.
- Hydration: Drink plenty of fluids to stay hydrated and aid in the healing process.
When to See a Dentist or Doctor
While most mouth ulcers are benign and self-limiting, there are certain situations where it is essential to seek professional help:
- Persistent Ulcers: If an ulcer lasts longer than two weeks without improvement, it could indicate an underlying condition that requires further evaluation.
- Severe Pain or Discomfort: If the pain is severe and interferes with daily activities, a healthcare professional can recommend stronger medications or treatments.
- Recurring Ulcers: Frequent recurrence of mouth ulcers may warrant an assessment to identify potential underlying causes or deficiencies.
- Accompanying Symptoms: If ulcers are accompanied by systemic symptoms such as fever, swollen lymph nodes, or significant weight loss, it’s essential to seek medical attention.
- Signs of Infection: If there are signs of infection, such as increased redness, pus, or fever, it’s crucial to consult a healthcare provider.
Conclusion
Mouth ulcers can be a painful and frustrating condition, but understanding their causes, symptoms, and treatments can help individuals manage them effectively. By practicing good oral hygiene, being mindful of dietary choices, and implementing self-care measures, most mouth ulcers can heal without the need for medical intervention. However, if you experience persistent, severe, or recurrent ulcers, do not hesitate to seek the advice of a dentist or healthcare professional for proper diagnosis and treatment.

