Arthritis is a chronic condition that affects millions of people, causing pain, stiffness, and reduced mobility in the joints. While lifestyle changes, medication, and physical therapy can help manage arthritis symptoms, some individuals may require more advanced treatments to improve their quality of life. In this article, we will explore some of the more intensive arthritis treatments, including corticosteroid injections, joint replacement surgery, and emerging therapies like stem cell therapy.
1. Corticosteroid Injections for Arthritis Pain Relief
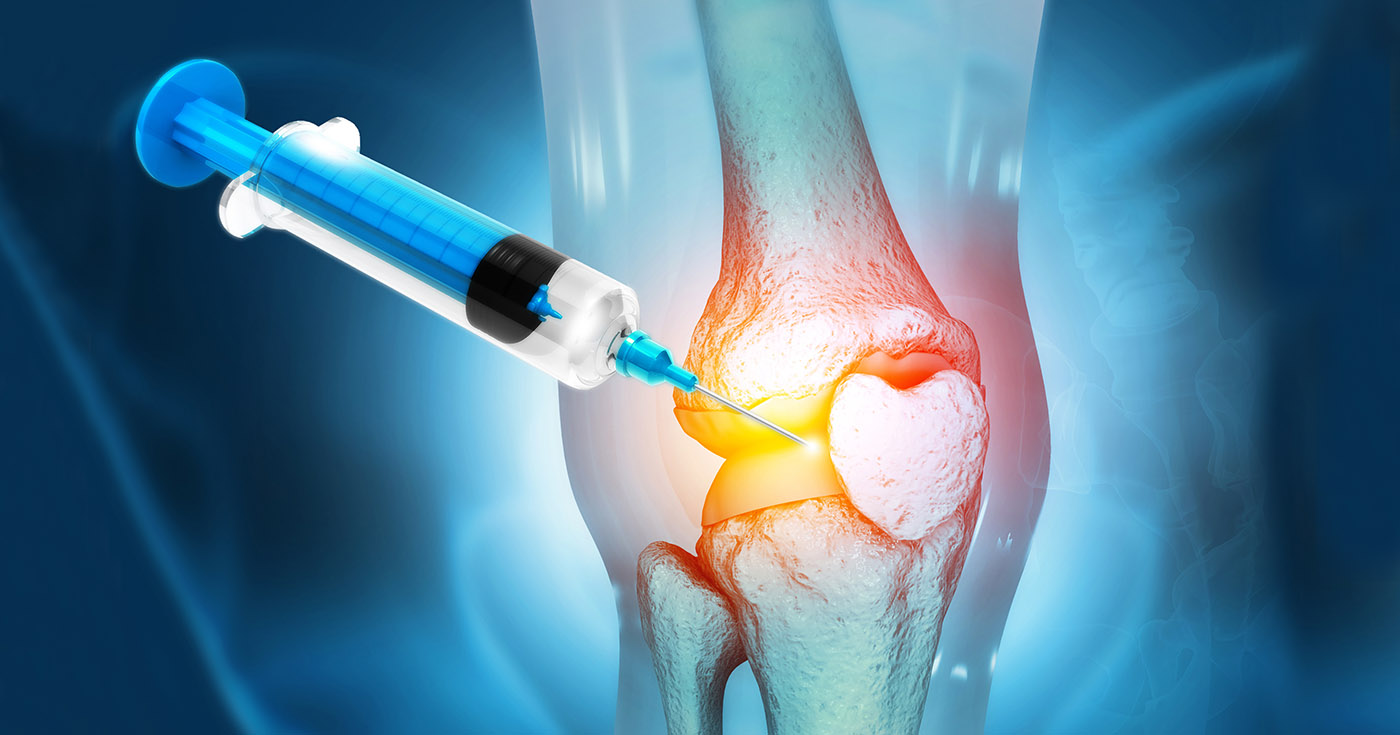
Corticosteroid injections are one of the most common advanced treatments used to manage arthritis symptoms, particularly for those with severe joint inflammation. These injections help reduce inflammation and provide relief from pain and swelling.
How Corticosteroid Injections Work
Corticosteroids are synthetic versions of cortisol, a hormone produced by the adrenal glands that helps control inflammation. When injected directly into an affected joint, these steroids can help suppress the immune system’s inflammatory response and provide significant relief from arthritis symptoms.
Benefits of Corticosteroid Injections
- Rapid Pain Relief: One of the primary benefits of corticosteroid injections is their ability to provide quick and effective pain relief, often within a few days of administration.
- Reduced Inflammation: The injection directly targets the inflamed area, reducing swelling and improving joint function.
- Temporary Relief: While corticosteroid injections do not cure arthritis, they can provide temporary relief, helping individuals manage their symptoms and improve mobility, especially during flare-ups.
Risks and Side Effects
While corticosteroid injections are generally safe, they are not without risks. Repeated injections can weaken the bones, cartilage, and tendons around the joint. Overuse can also increase the risk of infections, and in some cases, the injections may only provide short-term relief.
2. Joint Replacement Surgery
For individuals with severe arthritis who experience significant joint damage and debilitating pain, joint replacement surgery may be the best option. This procedure involves removing a damaged or arthritic joint and replacing it with an artificial joint made of metal, plastic, or ceramic materials.
When Is Joint Replacement Surgery Necessary?
Joint replacement is typically considered when other treatments, such as medications, physical therapy, and injections, have not provided sufficient relief. It’s most commonly performed for arthritis in weight-bearing joints like the hips, knees, and shoulders, but it can also be done for the fingers and elbows.
Types of Joint Replacement Surgeries
- Knee Replacement: One of the most common forms of joint replacement, where the damaged knee joint is replaced with a prosthetic.
- Hip Replacement: This surgery replaces a worn-out or damaged hip joint, relieving pain and improving mobility.
- Shoulder Replacement: If arthritis in the shoulder becomes severe, a partial or total shoulder replacement can restore movement and alleviate pain.
Benefits of Joint Replacement Surgery
- Long-Term Pain Relief: Joint replacement surgery can offer long-lasting relief from arthritis pain, enabling individuals to regain mobility and resume normal activities.
- Improved Functionality: The replacement joint can restore function to the affected area, significantly improving the quality of life for many patients.
- High Success Rate: Joint replacement surgeries have a high success rate, with most patients reporting significant improvements in pain and mobility.
Risks and Recovery
Like any major surgery, joint replacement comes with risks, including infection, blood clots, and complications related to anesthesia. Recovery time can vary but generally involves physical therapy to help the patient regain strength and movement in the new joint. While joint replacement is a highly effective treatment, it is usually considered a last resort after other options have been exhausted.
3. Stem Cell Therapy: A Promising Alternative
Stem cell therapy is an emerging treatment that has shown promise in treating arthritis, particularly for those with osteoarthritis or rheumatoid arthritis. This treatment uses stem cells to repair or regenerate damaged tissue and potentially reduce the need for more invasive procedures, such as surgery.
How Stem Cell Therapy Works
Stem cell therapy involves injecting stem cells (often derived from the patient’s own body, such as from bone marrow or adipose tissue) into the affected joint. These stem cells have the potential to develop into various types of cells, including cartilage and other connective tissues, which can help repair damage caused by arthritis.
Benefits of Stem Cell Therapy
- Regenerative Potential: Stem cells can help regenerate damaged cartilage, providing long-term relief and slowing the progression of arthritis.
- Reduced Inflammation: Stem cells may also help reduce inflammation in the joint, alleviating pain and improving mobility.
- Less Invasive: Compared to joint replacement surgery, stem cell therapy is a less invasive procedure with a quicker recovery time.
Risks and Considerations
While stem cell therapy holds great promise, it is still considered experimental in many cases and may not be covered by insurance. The long-term effectiveness of stem cell treatments for arthritis is still being studied, and not all patients are candidates for this therapy. It’s important to consult with a qualified healthcare provider to determine whether stem cell therapy is appropriate for your condition.
4. Platelet-Rich Plasma (PRP) Therapy
PRP therapy is another advanced treatment option that uses the patient’s own blood to help heal damaged tissues. During this procedure, blood is drawn from the patient, processed to concentrate the platelets, and then injected into the affected joint.
How PRP Therapy Works
Platelets are rich in growth factors that can stimulate tissue repair. By injecting concentrated platelets into an arthritic joint, PRP therapy aims to promote healing, reduce inflammation, and alleviate pain.
Benefits of PRP Therapy
- Promotes Healing: The growth factors in PRP can stimulate the body’s natural healing processes, improving cartilage regeneration and reducing inflammation.
- Non-Surgical: PRP therapy is a non-invasive procedure, making it an attractive alternative to surgery for some patients.
Risks and Effectiveness
While PRP therapy shows promise, its effectiveness in treating arthritis varies. Some patients experience significant relief, while others may not see the same level of improvement. Like other advanced treatments, it is important to discuss the potential risks and benefits with your doctor.
5. Other Advanced Arthritis Treatments
Other advanced treatments include:
- Surgery for Deformities: For some individuals with severe joint damage, corrective surgery may be necessary to address deformities caused by arthritis.
- Laser Therapy: Low-level laser therapy (LLLT) can help reduce pain and inflammation in affected joints.
- Viscosupplementation: In this procedure, hyaluronic acid is injected into the joint to lubricate it and reduce friction, which can help relieve pain in joints affected by osteoarthritis.
6. Conclusion
While traditional treatments like medication and physical therapy remain essential for managing arthritis, more advanced therapies offer additional options for those with severe symptoms or joint damage. Corticosteroid injections, joint replacement surgery, and stem cell therapy are all viable choices depending on the severity of the condition. As medical advancements continue, new treatments and techniques may further improve the quality of life for individuals living with arthritis. If you’re considering advanced treatment options, consult with your healthcare provider to discuss which approach is best suited to your needs.

