Diabetes is one of the most common chronic health conditions worldwide, affecting millions of people. Understanding the differences between Type 1 and Type 2 diabetes is crucial for effective management and care. In this blog, we’ll explore what sets these two types of diabetes apart, their symptoms, and some essential tips to help manage both types effectively.
What is Diabetes?
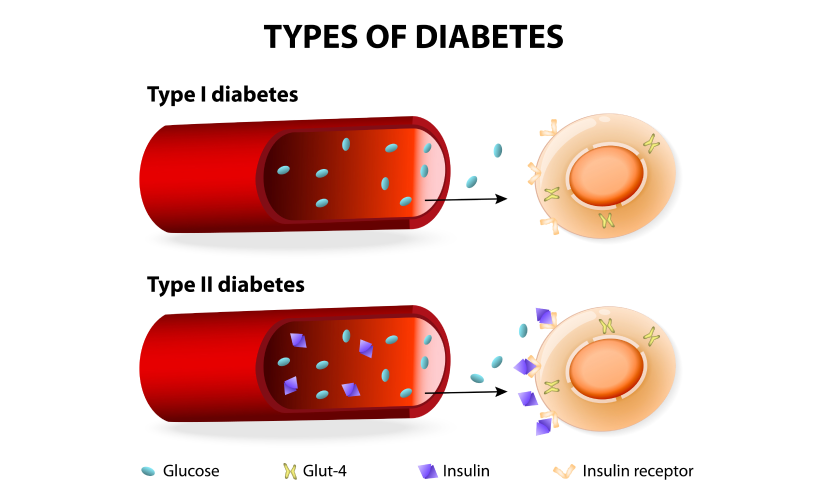
Diabetes is a metabolic disorder characterized by high blood sugar levels. It occurs when the body either doesn’t produce enough insulin or can’t use it effectively. Insulin is a hormone produced by the pancreas that helps regulate blood glucose levels. Without enough insulin or the ability to use it properly, blood sugar can reach dangerously high levels, leading to various health complications.
Key Differences Between Type 1 and Type 2 Diabetes
While both Type 1 and Type 2 diabetes involve high blood sugar levels, the underlying causes and characteristics of each type are quite different.
1. Type 1 Diabetes
- Cause: Type 1 diabetes is an autoimmune disease. The immune system mistakenly attacks and destroys the insulin-producing cells (beta cells) in the pancreas. As a result, the body is unable to produce insulin.
- Age of Onset: It is commonly diagnosed in children and young adults, though it can develop at any age.
- Prevalence: Type 1 diabetes is less common than Type 2, accounting for about 5-10% of all diabetes cases.
- Symptoms: The symptoms often develop quickly and may include extreme thirst, frequent urination, weight loss, fatigue, and blurred vision.
2. Type 2 Diabetes
- Cause: In Type 2 diabetes, the body either becomes resistant to insulin or doesn’t produce enough insulin to maintain normal blood glucose levels. This resistance is often linked to lifestyle factors, such as a high-calorie diet and lack of exercise, along with genetic predisposition.
- Age of Onset: While it was traditionally considered adult-onset diabetes, Type 2 diabetes is now increasingly diagnosed in children and adolescents due to rising obesity rates.
- Prevalence: Type 2 diabetes is the most common type, accounting for 90-95% of all diabetes cases.
- Symptoms: Symptoms develop gradually and may include increased thirst and hunger, frequent urination, fatigue, slow-healing sores, and frequent infections.
Symptoms of Type 1 and Type 2 Diabetes
Although some symptoms overlap, there are subtle differences in how each type of diabetes manifests:
| Symptom | Type 1 Diabetes | Type 2 Diabetes |
| Excessive Thirst | Common, often sudden | Common, develops gradually |
| Frequent Urination | Yes | Yes |
| Fatigue | Extreme | Common |
| Unintended Weight Loss | Common | Rare |
| Blurred Vision | Yes | Yes |
| Slow-Healing Wounds | Less common | Common |
| Frequent Infections | Less common | Common |
Causes and Risk Factors
Understanding the causes and risk factors for each type can aid in prevention (where possible) and early detection.
Type 1 Diabetes
- Genetics: A family history of Type 1 diabetes increases the risk.
- Autoimmune Response: It’s believed that environmental factors, like viral infections, might trigger the autoimmune response that destroys insulin-producing cells.
Type 2 Diabetes
- Lifestyle Factors: Poor diet, lack of physical activity, and being overweight or obese increase the risk.
- Genetics: A family history of Type 2 diabetes raises the risk.
- Age: While Type 2 can develop at any age, it’s more common in people over 45.
Management Tips for Type 1 and Type 2 Diabetes
Managing diabetes effectively is crucial for maintaining a healthy lifestyle and preventing complications. Here’s a guide to managing both types:
1. Insulin Therapy and Medication
- Type 1 Diabetes: Daily insulin injections are necessary since the body cannot produce insulin. Options include multiple daily injections or insulin pump therapy.
- Type 2 Diabetes: Lifestyle changes, oral medications, and sometimes insulin are used to control blood sugar. Medications like metformin can improve insulin sensitivity and lower blood glucose levels.
2. Dietary Management
- Low-Glycemic Foods: Both Type 1 and Type 2 diabetics should focus on foods with a low glycemic index, such as vegetables, whole grains, and legumes.
- Consistent Carbohydrate Intake: Maintaining a balanced carbohydrate intake helps stabilize blood sugar levels.
- Avoid Processed Sugars: Reduce intake of refined sugars, sugary drinks, and high-carb processed foods.
3. Regular Exercise
- Improving Insulin Sensitivity: Exercise can help cells become more sensitive to insulin, which is especially helpful for managing Type 2 diabetes.
- 30 Minutes a Day: Aim for at least 30 minutes of moderate exercise, like walking, swimming, or cycling, five days a week.
- Stay Hydrated: Drink plenty of water, especially during exercise, as dehydration can affect blood sugar levels.
4. Monitor Blood Glucose Levels
- Track Daily Levels: Regularly monitoring blood glucose is essential for both types to keep blood sugar within the target range.
- Continuous Glucose Monitoring (CGM): CGMs provide real-time data, making it easier for individuals to manage their levels throughout the day.
5. Manage Stress
- Mindfulness and Meditation: Stress can raise blood sugar levels, so practices like meditation and deep breathing can be beneficial.
- Adequate Sleep: Poor sleep can negatively affect blood glucose and insulin sensitivity.
6. Routine Check-ups
- Regular visits to your healthcare provider can help monitor your diabetes and catch any potential complications early.
Final Thoughts
Understanding the differences between Type 1 and Type 2 diabetes, along with their unique management needs, is essential for maintaining a high quality of life. Whether through lifestyle changes, medication, or regular monitoring, taking proactive steps to control blood sugar levels can reduce the risk of complications and help you lead a healthy life.
By following the right management strategies, you can live well with diabetes. Remember to work closely with healthcare professionals to create a personalized care plan that suits your individual needs.
By including specific keywords such as “Type 1 diabetes,” “Type 2 diabetes,” “diabetes symptoms,” and “diabetes management,” this blog is optimized to attract readers looking for information on both types of diabetes and their management.

